Symptoms | Diagnosis | Causes | Conservative Treatments | Surgical Treatment | Microsurgery and Supermicrosurgery | Consultation | FAQ
WHAT IS LYMPHOEDEMA AND WHICH PARTS OF THE BODY ARE AFFECTED?
The lymphatic system forms an integral part of the immune system and is made up of delicate lymphatic vessels and lymph nodes. Its main functions include the elimination of harmful cells and the transfer of white blood cells.
If this transport mechanism is impaired, it can lead to a condition known as lymphoedema.
Lymphoedema takes the form of visible and palpable swelling, which can occur on the arms, legs and/or trunk. However, swelling in these areas is not always lymphoedema. Consequently, an expert physical examination is very important.
Lymphoedema is a chronically progressive disease with the potential for disability.
Typical symptoms of lymphoedema are:
- Swelling, which usually occurs on the arms or legs
- A feeling of tightness, especially when wearing tight-fitting clothing
- Noticeable and long-lasting pressure marks on the skin
- Changes to the skin such as thickening or hardening
- Dull pain in the areas affected
- The appearance of small blisters that leak clear fluid
Lymphoedema can occur anywhere on the body, although it is usually more common on the arms or legs.
The symptoms develop gradually over weeks or months and, in cancer patients, can even occur years after cancer treatment.
The symptoms associated with lymphoedema can significantly impair daily activities. This can manifest itself, for example, in wearing unsuitable shoes or limited mobility.
In addition, patients have an increased risk of infections in the areas affected, as the lymphatic system is weakened at this point and the skin is more susceptible to tearing due to the swelling.
Early detection of lymphoedema is crucial in order to prevent or minimise the potential health complications of persistent congestion through appropriate treatment.
During the medical consultation and a physical examination, the specialist can determine whether lymphoedema is present and what stage it is at. It is also important to rule out other possible causes of swelling and discomfort.
The stages of lymphoedema
The onset of lymphoedema can vary from person to person, as the structure of the lymphatic system differs between individuals. There can even be differences within the lymphatic system, for example, in the number of lymphatic vessels on the right and left sides of the body.
This means that lymphoedema can have different manifestations, even if it is due to the same cause, such as surgery or radiotherapy.
A distinction is made between different stages of lymphoedema, to describe the severity of the disease: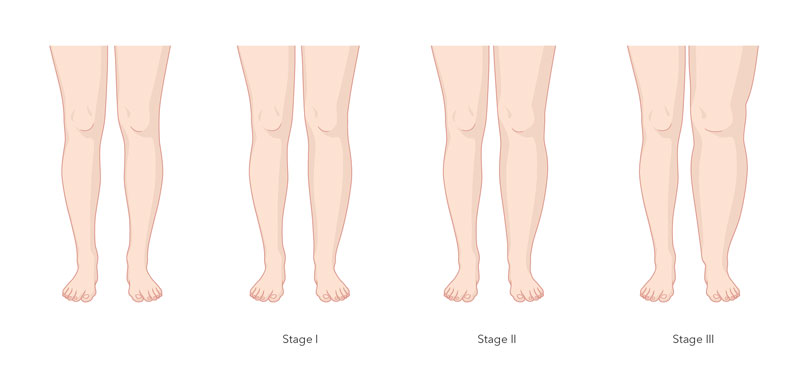
Stage 0
At this earliest stage, no oedema is visible or palpable. Nevertheless, there is a latent risk of developing lymphoedema, as the preconditions for this (damage caused by cancer surgery or radiation) are present. The duration of the latency stage is unpredictable; it can last for life or only a short time. No treatment is required at this stage, but precautionary measures should be taken.
Stage 1
At this stage, visible and palpable lymphoedema is present, which increases during the day and partially disappears overnight. Signs of this may be that clothes or jewellery fit tighter in the evening or leave marks. If these symptoms occur, it is advisable to consult a doctor, who can then arrange a referral for physiotherapy. In this phase, a few therapeutic measures are often enough to slow down the progression of the disease.
Stage 2
In stage 2, the lymphoedema persists overnight and is permanently visible and palpable. However, it need not be very pronounced. At this stage, manual lymphatic drainage is necessary. This is performed by a physiotherapist.
Stage 3
At this advanced stage, not only is permanent swelling visible but also complications such as skin changes (colour and appearance), and there may be inflammation and considerable limitations in everyday life. Treatment at this stage is complex, but can also reduce major lymphoedema with complications. This leads to an improvement in the person’s overall health.
The examination process
Advanced procedures are available to visualise and examine the lymphatic vessels:
- Examination of the vascular system (angiology)
- Ultrasound
- Oscillography (blood pressure measurement in the legs)
- Volumetry (measuring the volume of the legs)
- Lymphoscintigraphy (diagnostic imaging)
- Indocyanine green lymphangiography (visualisation of the lymphatic vessels)
These procedures play a particularly important role in the decision-making process when deciding whether surgical treatment is necessary.
Lymphoedema occurs when the lymph is no longer removed effectively via the lymphatic vessels between the cells – usually resulting in a backlog and the fluid collecting under the skin.
Oedema can also be caused by impaired heart or kidney function. Problems in the venous system or the use of certain medications can also lead to oedema.
WHAT TYPES OF LYMPHOEDEMA ARE THERE?
There are two main types of lymphoedema: primary and secondary lymphoedema, and secondary lymphoedema is more common than primary lymphoedema.
Primary lymphoedema
Primary lymphoedema, also known as congenital lymphoedema, is caused by the lymphatic system not developing adequately. This can occur in different parts of the body or it can be limited to a specific area.
In most cases, even if the lymphatic system is not adequately developed, sufficient lymph can be removed over a long period of time, so lymphoedema only occurs after several years.
Oedema can develop as a result of wound healing after an accident and may not completely resolve. In these cases, it is assumed that the lymphatic system was not fully functional from the beginning, which is why this oedema is also considered primary lymphoedema.
Primary lymphoedema can be present from birth, although this is rarely the case. It often develops as a reaction to a trigger, which can often only be identified via thorough examination.
However, it can also occur without a recognisable trigger, and its onset is not age-dependent. Typically, the legs are affected, and sometimes all of one side of the body.
Secondary lymphoedema
Secondary lymphoedema is an acquired condition that is often associated with cancer.
Cancer surgery in which lymph nodes were removed and/or radiation was required result in local damage to the lymphatic system that cannot be cured. Lymph nodes have no regenerative capacity, so the lymphatic system may no longer be able to drain all of the lymphatic fluid from the affected tissue.
The lymphatic system is structured in such a way that the lymph flows from an arm or leg into the central lymph nodes in the corresponding section of the trunk. The effects of a lymphatic system disorder can only be seen in this specific area of the body.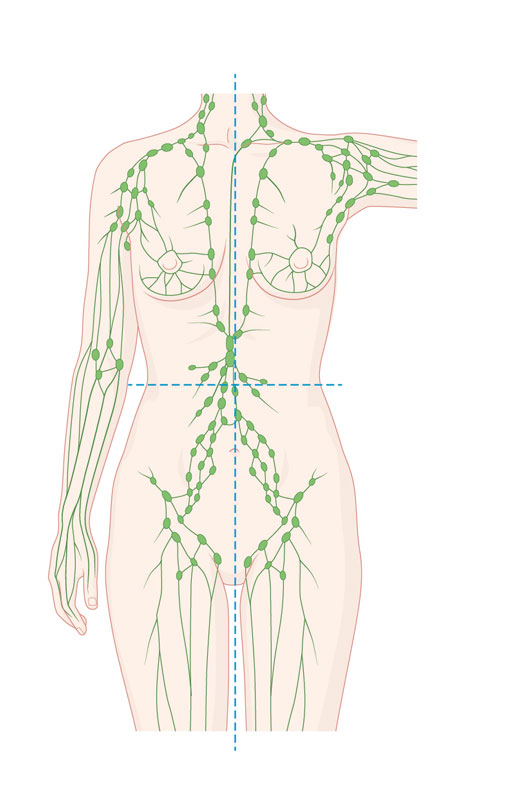 For example, after surgery to remove a tumour from the left breast, lymphoedema can occur in the left arm and/or the left part of the trunk, but not in the right arm or leg. Similarly, damage to the lymphatic system caused by the treatment of an abdominal tumour can never lead to lymphoedema in an arm.
For example, after surgery to remove a tumour from the left breast, lymphoedema can occur in the left arm and/or the left part of the trunk, but not in the right arm or leg. Similarly, damage to the lymphatic system caused by the treatment of an abdominal tumour can never lead to lymphoedema in an arm.
In some cases, especially in people with a high number of lymphatic vessels, lymphoedema may never occur despite cancer surgery with lymph node removal and radiotherapy. Studies on women after breast cancer have shown that only around one in five develop arm lymphoedema over time.
Secondary lymphoedema can develop immediately after cancer treatment or years later. This depends on the duration of the compensation mechanisms. It is important to emphasise that lymphoedema does not have to be an inevitable consequence of cancer therapy.
It is important to emphasise that lymphoedema does not have to be an inevitable consequence of cancer therapy.
WHAT IS THE AIM OF THE TREATMENT?
It is not usually possible for lymphoedema to heal completely.
Treatment focuses on controlling the swelling, improving the functionality of the limbs affected and preventing complications such as infection. In many cases, lifestyle changes are essential for sustainable improvement.
As part of their physiotherapy, people affected are given instructions on massage techniques and special exercises that support the drainage of lymphatic fluid. Compression stockings may also be recommended. These stockings apply gentle pressure to the affected leg or arm, which distributes the accumulated fluid more evenly and allows it to be removed more efficiently by the lymphatic system.
The combination of manual lymphatic drainage and compression therapy is the gold standard in the conservative treatment of lymphoedema.
Surgical treatment is only considered after at least one year of conservative physiotherapy. Patients with secondary lymphoedema must also be cancer-free for at least one year. If this is the case, a specialist can assess whether a surgical procedure would be promising, and which technique should be used.
The surgical treatment of lymphoedema comes under the umbrella of plastic surgery. Thanks to major advances in surgical techniques, the following four procedures are now available:
- Vascularised lymph node transfer (VLNT)
- Vascularised lymph vessel transfer (VLVT)
- Lymphovenous anastomosis (LVA)
- Liposuction
These procedures can greatly improve the quality of life of people affected. They are performed by our experienced specialist, Professor Mario Scaglioni .
TWO KEY APPROACHES IN THE SURGICAL TREATMENT OF LYMPHOEDEMA
- Removal of excess tissue
- Improvement of lymphatic drainage
Reconstructive measures include techniques such as lymphovenous anastomosis (LVA), vascularised lymph node transfer (VLNT) and vascularised lymph vessel transfer (VLVT). Microsurgery procedures using high-precision instruments and powerful microscopes make it possible to treat tiny lymphatic vessels. This involves connecting healthy lymphatic vessels with other small lymphatic or blood vessels in order to bypass blockages and normalise lymph flow.
Other procedures that are available include liposuction, in which excess fatty tissue is removed using blunt, vibrating cannulas. This procedure can effectively help to reduce the size of the swollen arms or legs. Nevertheless, the use of compression therapy after surgical treatment is still essential.
With the help of microsurgery and supermicrosurgery, it is possible to restore the lymph flow.
Lymphatic surgery is an essential component of cancer treatment. It not only has high diagnostic value but is also considered the gold standard of many oncological treatment concepts.
As a complication of these treatments, lymphoedema remains a challenging clinical problem. Lymphoedema of the lower limbs is far more common than lymphoedema of the upper limbs, which is mainly associated with breast cancer and its treatment.
The treatment of lymphoedema is complex. However, an increased understanding of the lymphatic system and the use of microsurgery and supermicrosurgery have opened up new ways of treating lymphoedema.
Supermicrosurgery makes it possible to dissect the smallest lymphatic vessels with a diameter of 0.3 to 0.8 mm and restore their flow. The finest surgical instruments and a microscope with up to 40x magnification are used.
The techniques described below can be used to reconstruct the lymphatic drainage.
CREATING NEW LYMPHATIC CHANNELS WITH LYMPHOVENOUS ANASTOMOSIS (LVA)
Lymphovenous anastomosis (LVA) provides for passage of fluid via the creation of new, extra-anatomical lymphatic channels.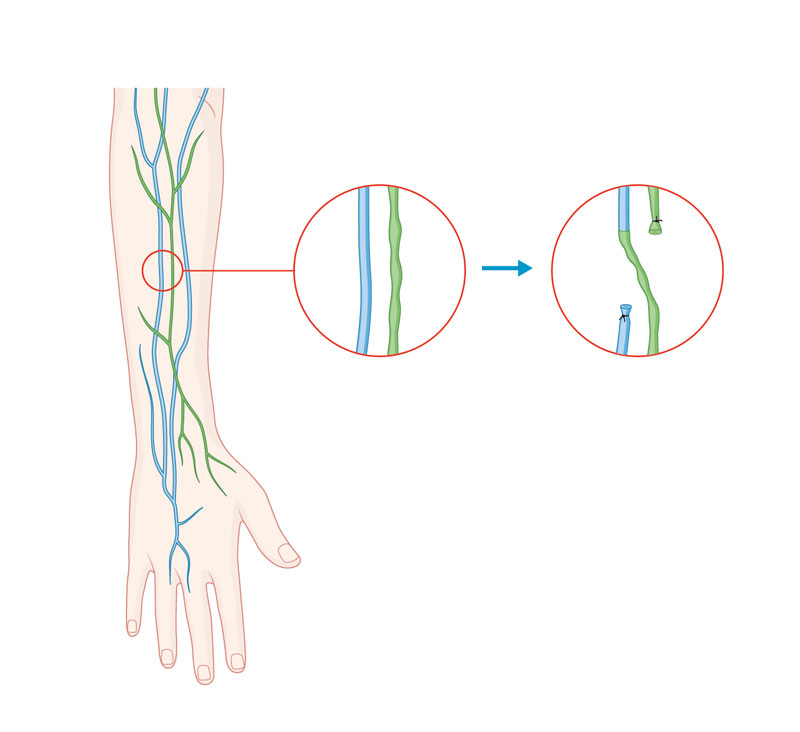 To preoperatively locate the lymphatic system, we inject a dye known as indocyanine green (ICG) to provide mapping of the insufficient lymphatic vessels.
To preoperatively locate the lymphatic system, we inject a dye known as indocyanine green (ICG) to provide mapping of the insufficient lymphatic vessels.
The lymphatic vessels that are still active are then connected via anastomosis to veins of the same calibre in order to restore the continuity of lymphatic drainage. It is also possible to connect lymphatic vessels directly to other surrounding lymphatic vessels.
In the affected limbs, reductions in size of almost 40% and equally significant skin improvements can be achieved.
This unique supermicrosurgical technique requires many years of experience in microsurgery and the use of highly specialised instruments. This surgical method is no longer available in advanced stages of the disease.
TRANSPLANT OF HEALTHY LYMPH NODES VIA VASCULARISED LYMPH NODE TRANSFER (VLNT)
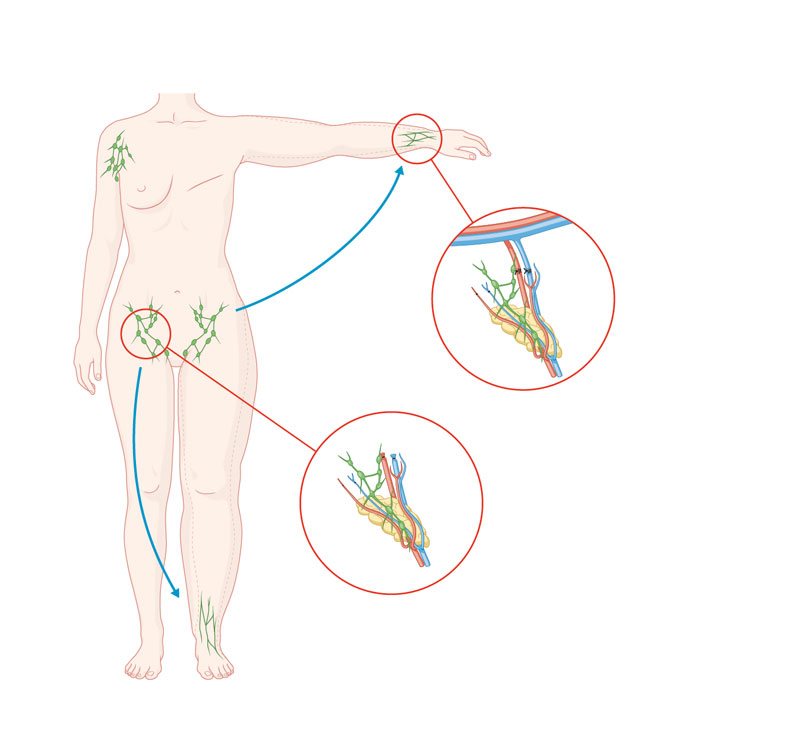 Lymph node transfer involves the removal of lymph nodes from a healthy region of the body, for example, from the groin or collarbone area. These lymph nodes are removed together with the associated blood vessels and the surrounding fatty tissue and then transferred to the affected limb. The blood vessels are microsurgically connected to the vascular system of the target area to ensure efficient blood flow to the transferred lymph nodes.
Lymph node transfer involves the removal of lymph nodes from a healthy region of the body, for example, from the groin or collarbone area. These lymph nodes are removed together with the associated blood vessels and the surrounding fatty tissue and then transferred to the affected limb. The blood vessels are microsurgically connected to the vascular system of the target area to ensure efficient blood flow to the transferred lymph nodes.
The transferred lymph nodes are able to absorb lymphatic fluid from their surroundings and drain it via the blood vessels. New lymphatic channels can also be formed over the long term. Lymph node transfer not only reduces the oedema but also improves the local immunological situation. As a result, inflammation such as erysipelas rarely occurs.
This procedure can reduce the extent of oedema by 60 to 80% in the long term and significantly reduce the frequency of infections. However, it is important to note that it can take around a year for the full success of the procedure to become apparent. Despite this limitation, this procedure can also be performed for advanced and long-standing lymphoedema.
TRANSFER OF LYMPHATIC TISSUE VIA VASCULARISED LYMPHATIC VESSEL TRANSFER (VLVT)
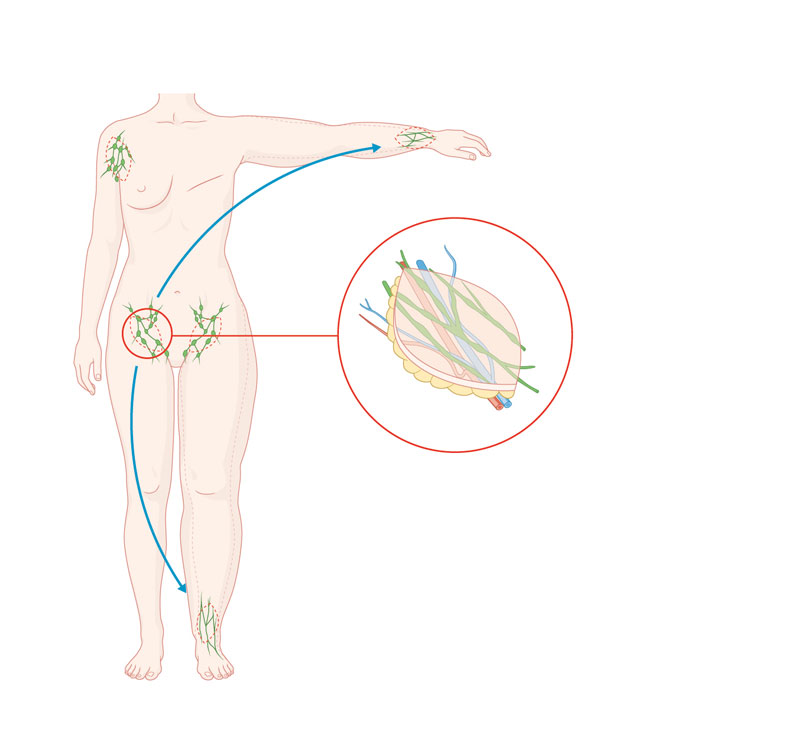 Alternatively, it is possible to restore the lymph flow in the limbs affected using a flap technique. A free or pedicled flap with lymphatic vessels acts as a lymphatic ‘bridge’.
Alternatively, it is possible to restore the lymph flow in the limbs affected using a flap technique. A free or pedicled flap with lymphatic vessels acts as a lymphatic ‘bridge’.
This treatment option uses spontaneous regeneration or reconnection of lymphatic vessels after a part has been replaced by the lymphatic bridge. The restoration of lymphatic vessels after free tissue transfer has been confirmed in lymphoscintigraphic studies (imaging).
All of these diagnostic and therapeutic procedures require sophisticated techniques and instruments that are only offered in a few centres in Europe. We are the only hospital in the Zurich area to offer preoperative lymphatic vessel diagnostics and reconstructive lymphatic vessel surgery.
WHAT FOLLOW-UP TREATMENT IS REQUIRED?
The follow-up treatment depends on the type of procedure, stage of the lymphoedema and individual needs of the patient.
Ideally, the follow-up treatment will include the following areas:
- Compression therapy: Wearing compression stockings or sleeves can help to support lymph flow and reduce swelling.
- Physiotherapy: Physiotherapy exercises and manual lymphatic drainage techniques support mobility, lymphatic drainage and control of swelling.
- Lifestyle changes: Individuals can be instructed to maintain a healthy diet, control their weight and exercise regularly to support the health of the lymphatic system.
- Monitoring: Regular medical examinations are needed to monitor progress and adjust the treatment strategy if necessary.
Lymphoedema is a chronic disease. Accordingly, certain risk factors must be taken into account – including after surgery. Experience has shown that heat (e.g., sauna), prolonged and strenuous physical exertion and too many knocks or bumps can have particularly negative effects on lymphoedema.
Technically challenging procedures such as lymphoedema treatment should always be carried out by experienced specialists. This enables the complication rate to be reduced to an absolute minimum.
Our specialist in lymphoedema treatments, Professor Mario Scaglioni, has many years of experience and a high level of expertise in lymphatic surgery.
In particular, the latest surgical techniques based on microsurgery and supermicrosurgery, performed by Professor Mario Scaglioni, offer new treatment options for even better results.
Our specialists are a well-coordinated team that will take care of you and your health comprehensively, expertly and personally. Contact us online or by phone to arrange your individual appointment.
What actions can I take that will help with my lymphoedema?
Maintaining a healthy lifestyle is crucial, as sufficient physical activity and a balanced diet can help to improve symptoms. Being overweight can aggravate the symptoms and should therefore be avoided. In addition, elevating the affected arm or leg while sitting or lying down can be helpful to support lymphatic drainage.
It is important to note that the affected area is more susceptible to infection. Because of this, it is essential to use skin-friendly moisturisers and sun protection to care for the skin, prevent cracks and maintain the skin’s protective function. Likewise, even the smallest injuries should be avoided, for example, by taking extra care when shaving or nail clipping to minimise the risk of infection in the area.
What sports are suitable for people with lymphoedema?
Special exercises that can be learned in physiotherapy are particularly important. Gentle sports are also recommended, such as water sports, cycling, yoga or Nordic walking. Regular muscle activity provides a form of massage for the limbs affected.
Can I go on holiday or to a spa if I have lymphoedema?
Yes, you can definitely travel, but there are some important considerations to take into account. It is best to move your legs repeatedly during the journey. Wearing compression stockings is particularly recommended for longer periods of sitting, such as during air travel. It should also be noted that heat can aggravate lymphoedema and damage the skin. So it is advisable to avoid travelling to hot regions, avoid extensive sunbathing and limit visits to saunas.