Injuries to the cruciate ligament | Cruciate ligament tears
Causes | Symptoms | Diagnosis | Treatments | Consultations & second opinions
What is a tear to the knee ligaments?
The knee joint is the largest joint in the human body and has a complex arrangement of ligaments. The four most important are the anterior cruciate and posterior cruciate ligaments, and the medial collateral and lateral collateral ligaments. When a knee ligament is torn, there is damage to one or more of these ligaments. Other structures in the knee may also be injured (for example, the meniscus).
What is the function of the cruciate ligaments?
The cruciate ligaments are one of the most important features providing central stability to the knee joint. They connect the femur (thigh bone) to the tibia in the lower leg. The knee has one anterior (front), and one posterior (rear), cruciate ligament. These cross in the centre of the knee joint.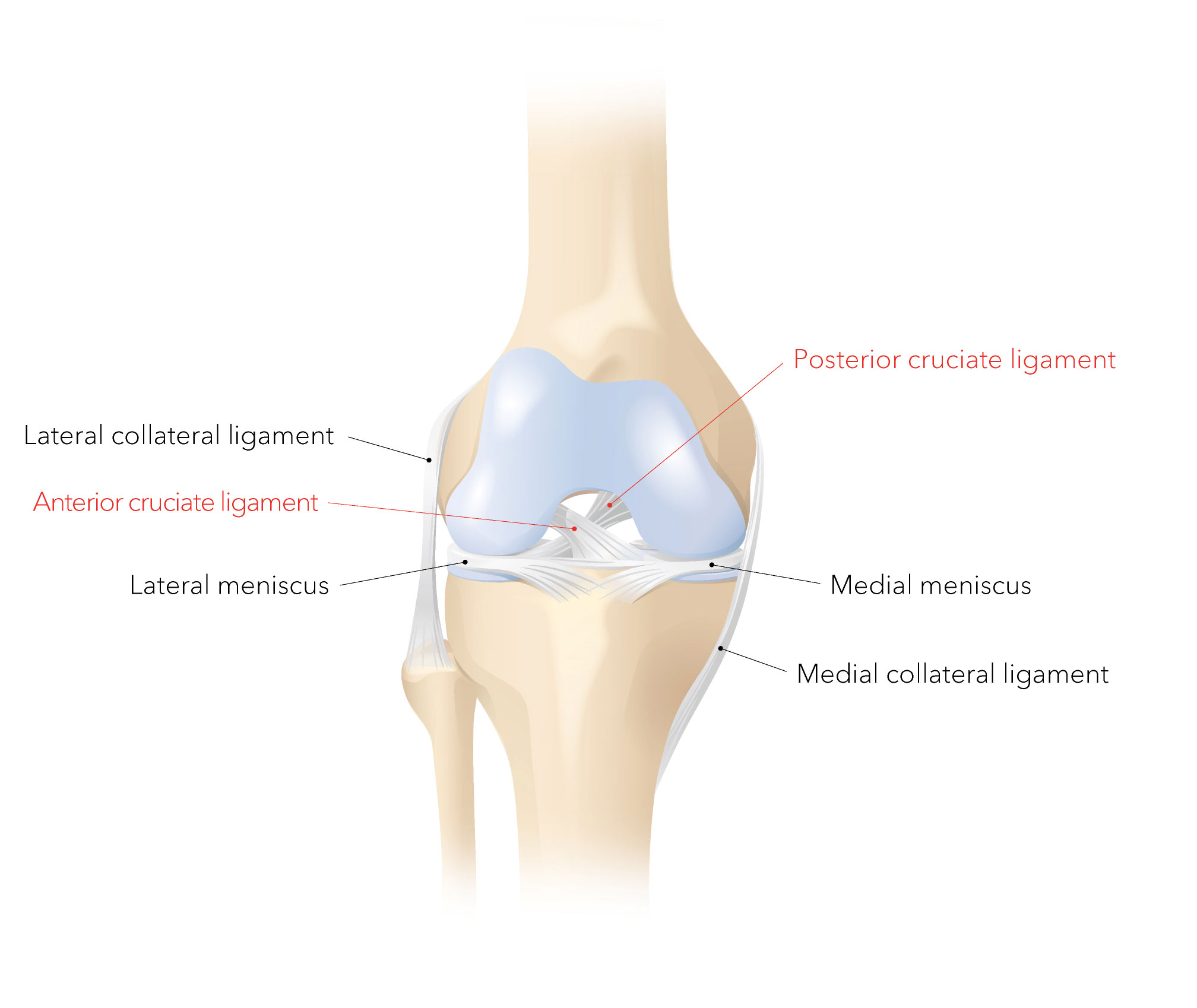
A cruciate ligament can tear when it is injured in an accident, for example, while skiing or playing football. In the case of the anterior cruciate ligament, this happens when the knee joint is bent and rotated while the lower leg is not moving. The anterior cruciate ligament is a bundle of fibres about 2 to 3 cm long and is the thickness of a little finger. In most cases (approx. 90%) it is the anterior cruciate ligament that tears (ACL tear or rupture).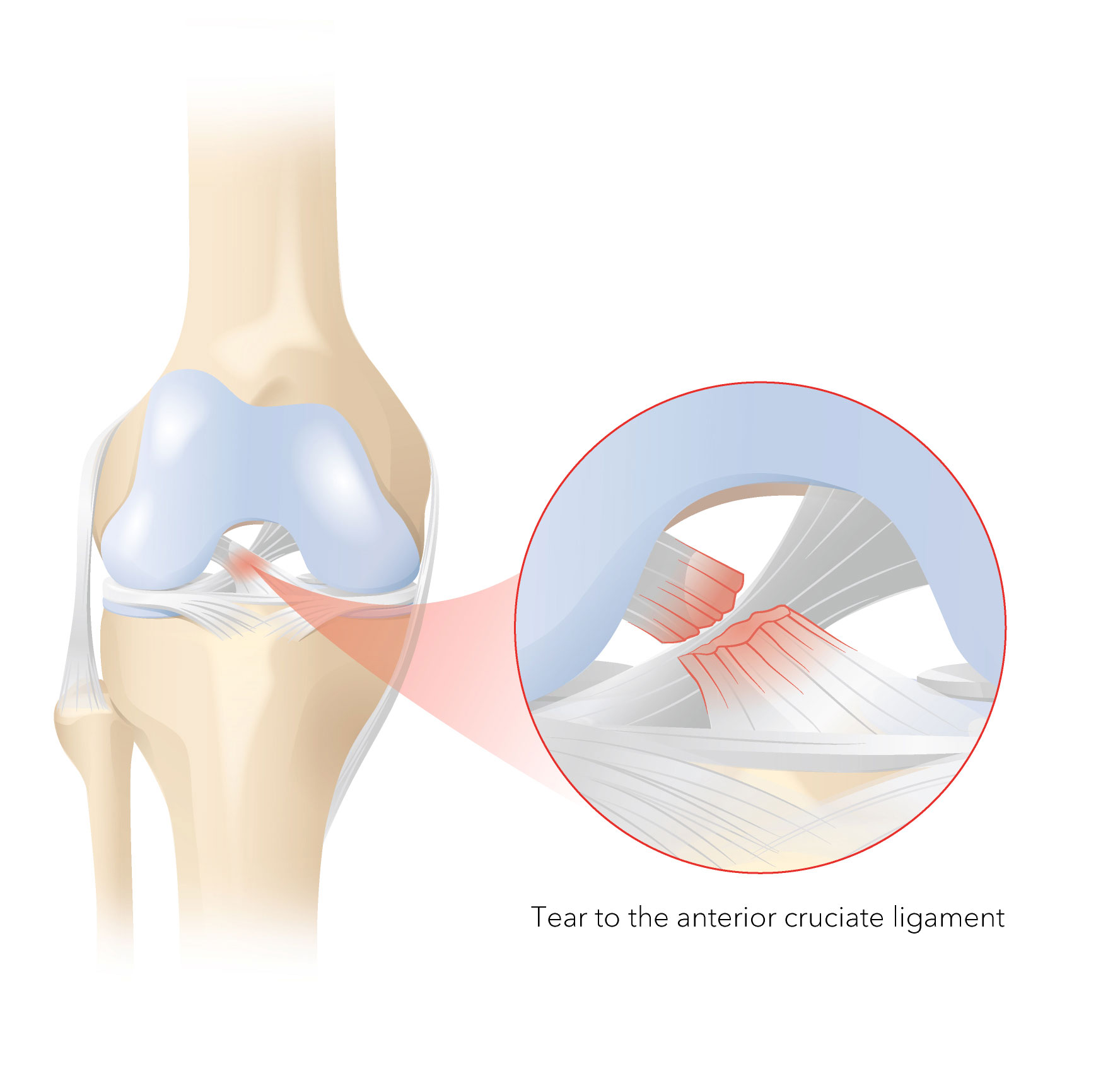
Tearing of the anterior cruciate ligament is usually accompanied by an audible crack, followed by temporary pain and swelling of the joint, with a resulting restriction in movement and weight bearing. This is caused by the nerve fibres and blood vessels running through the cruciate ligament. When the cruciate ligament is torn, the nerve fibres cause the pain and the torn blood vessels trigger bleeding into the joint. The person affected usually notices the instability in the knee joint immediately afterwards or once the acute pain symptoms or swelling around the knee have subsided. The knee joint buckles or “gives way” in an uncontrolled manner.
What are the consequences of a cruciate ligament tear?
A tear to the anterior cruciate ligament results in abnormally increased freedom of movement in the knee joint. In order to decrease this additional mobility, the existing structures in the knee joint such as the meniscus and the cartilage are put under significantly more stress. This extra strain can lead to long-term damage such as meniscus tears and wear on the cartilage (osteoarthritis of the knee).
Clinical examination assesses the instability of the knee joint by testing how far the lower leg can be moved relative to the thigh. The knee joint is also examined to see whether additional and specific pain can be triggered.
An MRI scan (magnetic resonance imaging) gives further information about the cruciate ligament tear as well as any accompanying injuries such as tears of the collateral ligament or meniscus and cartilage damage.
How is a torn ligament treated?
A cruciate ligament tear can be treated conservatively or surgically. The method chosen depends on the individual’s age and needs (e.g. if they play sport or have particular demands as part of their job) as well as on the type and location of the cruciate ligament tear and its accompanying injuries (e.g. additional tear of the meniscus). Any previous damage to the knee joint (cartilage damage, osteoarthritis of the knee) is also considered.
If only the cruciate ligament is torn and further accompanying injuries (meniscus tear) can be ruled out, and if the demands in terms of the person’s sports and job are very low, the cruciate ligament tear can be treated conservatively. Physiotherapy is used to strengthen the muscles and thus stabilise the knee joint.
If the knee joint remains insecure and unstable despite physiotherapy and the person affected is no longer able to cope in everyday life, surgical repair should be considered.
Surgical treatment
The more active a person is, and the younger they are, then the sooner the torn cruciate ligament should be treated surgically so as to avoid possible resultant damage (meniscus tear, osteoarthritis of the knee). Nowadays, there are several minimally invasive methods (such as arthroscopy) to repair a torn cruciate ligament. We make a distinction between surgery to preserve the cruciate ligament and surgery to replace it.
Cruciate ligament-preserving surgery
Surgery to preserve the cruciate ligament can be performed if the cruciate ligament is torn away directly at or close to the femur. In such cases, the torn cruciate ligament can be splinted with a strong thread and thus reattached to the point of origin (an internal brace, see image). This allows us to stabilise the cruciate ligament. In addition, a stitch is put in the torn cruciate ligament (a cruciate ligament suture) in order to promote self-healing of the cruciate ligament.
Accompanying injuries (e.g. meniscus tear, cartilage damage) can be treated during the same surgery. This suture and the splinting of the torn cruciate ligament are performed in a minimally invasive way using arthroscopy, thus supporting self-healing of the torn cruciate ligament. This innovative surgical technique delivers a stable result, allowing for early functional, aggressive post-operative treatment to start straight away with only temporary need for a knee support.
This cruciate ligament-preserving surgery should take place within three weeks of the accident, because after this point the torn cruciate ligament has shrunk too much.
Facts and figures
![Operation]()
Operation
Surgery time of around 60 minutes | Under general or regional anaesthetic
![Operation]()
Length of stay at the clinic
Clinic stay of approximately 3 days
![After the treatment]()
After the treatment
Post-operative treatment requires use of a walking stick for 2 weeks, wearing a knee support and undergoing intensive physiotherapy for approximately 3 months; full weight bearing is possible and knee has unrestricted mobility.
![Back to work]()
Back to work
For office-based jobs, you will be unable to work for approximately 2 weeks. This increases to 6 to 8 weeks for jobs involving strenuous physical activity.
![Sport]()
Sport
You will be able to take part in sports that are easy on the knee joint such as swimming, cycling, general exercise etc., approximately 3 months after surgery; for contact sports such as football or stop/start sports like tennis you should wait until approximately 6 months after surgery.
![Risk]()
Risk
Possible risks include general complications of surgery such as postoperative bleeding, infection, thrombosis, nerve injury (numbness, paralysis) and injury to vessels and soft tissue. Specific complications include limitations in movement of the knee joint, a feeling of instability and pain (e.g. excessive scarring of the knee joint with resulting restriction in movement and pain (arthrofibrosis), scarring of the cruciate ligament (cyclops syndrome), tearing of the ligament anchoring, overstretching or tearing of the cruciate ligament or suture).
Cruciate ligament replacement surgery (cruciate ligament reconstruction)
Reconstruction of the torn anterior cruciate ligament (ACL tear)
In cruciate ligament replacement, the disabled, torn cruciate ligament is removed and, in most cases, replaced by a tendon from your own body. In exceptional cases, an artificial cruciate ligament may also be used.
Surgery takes place either within 24 hours of the accident or two to four weeks after the injury. Swelling around the knee and bruising should have healed. In addition, mobility of the knee joint should have improved.
Cruciate ligament reconstructive surgery is highly demanding for the surgeon. We use what is known as the bone-tendon-bone technique, which is a common procedure and means that the new cruciate ligament graft taken from the patient consists of a bone fragment, a strip of tendon and a second bone fragment. The surgeon extracts a middle section of the patellar tendon with the corresponding bone fragments, one from the top of the tibia and one from the kneecap. These bone blocks heal into the insertion sites of the former cruciate ligament. Regrowth of the bone fragments takes about six weeks. To ensure stability early on and before regrowth, the bone fragments are secured with screws (some of which are dissolvable), sutures and special metal plates or clips.
Most of the surgery is performed arthroscopically, which is minimally invasive. Only the removal of the new cruciate ligament graft itself requires an additional incision to be made along the patellar tendon. This incision can also be used to open the knee joint (known as the “mini open” technique). Any accompanying injuries (e.g. meniscus tear, cartilage damage) can be treated at the same time.
This technique enables early functional, aggressive post-operative treatment. It is important to have good physiotherapy in place and to have a specific goal to aim for in your rehabilitation. Regular follow-up checks are also carried out by the surgeon. It will usually be possible to resume light sporting activities (e.g. cycling) after three months. Contact sports or sports with a lot of stop/start motion are not recommended for at least six months, depending on the condition of the muscles.
Reconstruction of a torn posterior cruciate ligament (PCL tear)
The surgical technique for reconstruction of the posterior cruciate ligament, which tears less frequently, is similar to that for the more frequently affected anterior cruciate ligament as described above. The posterior cruciate ligament is longer, thicker and more stable than the anterior cruciate ligament and prevents the lower leg from falling backwards relative to the thigh. The posterior cruciate ligament can tear when a large amount of direct force is applied to the bent knee.
The surgical procedure is significantly greater and more complex. Since the posterior cruciate ligament is longer than the anterior cruciate ligament, we do not use the patient’s own patellar tendon as a replacement. Instead, we use tendons from the inner side of the knee (the semitendinosus and gracilis tendons) or the quadriceps tendon. The new graft needs to be longer and thicker. It is inserted arthroscopically after drilling of the femur and tibia at the original insertion sites of the posterior cruciate ligament and fixed with screws (which are dissolvable) and clips.
In contrast to anterior cruciate ligament reconstruction, the post-operative treatment is very cautious. The operated knee must not bear weight or be actively bent for six weeks. In addition, the patient must wear a special knee brace, known as a PTS (posterior tibial support) brace for six weeks. The PTS brace contains padding that pushes the lower leg forward compared to the thigh. From the sixth week onwards, a special posterior cruciate ligament brace is worn for a further six weeks during the daytime.
Facts and figures
![Operation]()
Operation
The procedure takes around 90 minutes
![Operation]()
Length of stay at the clinic
Clinic stay of approximately 5 days
![After the treatment]()
After the treatment
Post-operative treatment requires use of a walking stick for 2 weeks, wearing a knee support and undergoing intensive physiotherapy for approximately 3 to 6 months, no kicking movements for 6 weeks; full weight bearing is possible and unrestricted mobility of the knee.
![Back to work]()
Back to work
For office-based jobs, you will be unable to work for approximately 3 to 6 weeks. This increases to 2 to 3 months for jobs involving strenuous physical activity.
![Sport]()
Sport
You will be able to take part in sports that are easy on the knee joint such as swimming, cycling, general exercise etc. approximately 3 months after surgery; for contact sports such as football or stop/start sports like tennis you should wait until approximately 6 months after surgery.
![Risk]()
Risk
Possible risks include general complications of surgery such as postoperative bleeding, infection, thrombosis, nerve injury (numbness, paralysis) and injury to vessels and soft tissue. Specific complications include limitations in movement of the knee joint, a feeling of instability and pain, e.g. excessive scarring of the knee joint with resulting restrictions in movement and pain (arthrofibrosis), scarring of the cruciate ligament graft (cyclops syndrome), tearing of the ligament anchoring, overstretching or tearing of the cruciate ligament or suture, suboptimal location of the new cruciate ligament graft, or the graft becoming jammed at the femur during extension (cruciate ligament graft impingement).
Our doctors have many years of experience and are highly skilled in sports and joint surgery. Dr Andreas L. Oberholzer is a well-known expert in knee surgery and has extensive experience in knee replacements. He trains international doctors in this area and promotes the further development of soft tissue-oriented techniques for implantation of artificial knee joints. You can find out more about his work here.
We guarantee rapid, expert assessment and consultation and treatment in line with the latest medical findings. Don’t hesitate to get in touch if you would like a second opinion.