Causes and symptoms | Diagnosis | Conservative and surgical treatments | Chronic pain | Artificial disc replacement | Consultations & second opinions
WHAT IS THE FUNCTION OF INTERVERTEBRAL DISCS?
Intervertebral discs provide for the mobility of the spine and act as a buffer between the vertebrae. An intervertebral disc consists of an elastic ring of firm, fibrous connective tissue (fibrous ring) and a soft core of gelatinous fluid (gelatinous core). Factors such as the natural ageing process and a lack of exercise alter the intervertebral discs. They lose fluid. This decreases their resistance, making them weaker and more vulnerable.
HOW CAN YOU RECOGNISE A SLIPPED DISC?
A slipped, herniated or prolapsed disc can be a cause of lower back pain. This occurs most frequently in adults between 30 to 50 years of age. Symptoms usually first appear in the lower back and leg and are aggravated by coughing or sneezing. Depending on the height of the slipped disc, loss of normal sensation often occurs, with numbness, tingling, formication or burning in the area supplied by the nerve.
A slipped or prolapsed disc is a result of degeneration and destruction of the disc’s fibrous outer ring and gelatinous core Chronic stress on the disc, lack of regenerative capacity of the tissue due to age, or injury of the cartilage plates of the adjacent vertebral bodies can lead to decline of the disc tissue. The lack of blood supply in the disc then inevitably leads to a process of degeneration. Inflammatory substances damage the disc and promote a cascade of degradation of the tissue. This leads to tears in the fibrous outer ring which, under pressure, allow part of the fibrous ring or the soft core of the disc to push outwards, presenting itself as a disc herniation or prolapse..
A slipped or herniated disc can be reliably detected via radiological imaging. An X-ray of the spine can be used to determine whether the height of the intervertebral discs has been reduced, i.e., whether the vertebral bodies are closer together or have moved. However, the suspicion of a slipped disc can be verified via magnetic resonance imaging of the affected spinal tract.
The treatment for a slipped or herniated disc always depends on the symptoms. If the pain is severe or lasts longer than three to four days, a doctor should be consulted. If additional signs of paralysis, numbness or tingling develop in the arms or legs, medical attention should be sought immediately in order to avoid permanent damage.
Convervative treatment
Surgical treatment
- Soft-tissue-sparing and minimally invasive surgical techniques
- Tissue removal by radiofrequency therapy
- Artificial disc replacement
If there is no indication of nerve damage in the form of abnormal sensation, numbness or paralysis of the arms, hands, legs or feet, conservative treatment over several months is recommended. If there is no permanent improvement of symptoms and pain after this period, however, surgical treatment is usually unavoidable. Indications for surgery include paralysis, numbness or tingling in the hands or feet, severe, non-treatable pain and acute bladder and/or rectal paralysis.
WHAT HAPPENS DURING DISC SURGERY?
Slipped or prolapsed discs most commonly occur within the lumbar spinal canal. They displace the nerve root posteriorly into the middle or lateral portion of the spinal canal (paramedian disc herniation). A small bone incision is made using an ultrasonic bone scalpel. Through the opening of the ligamentum flavum, the portion of the disc pressing on the nerve root is carefully removed.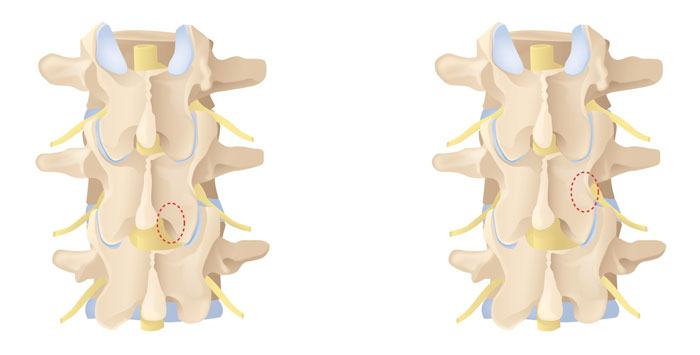
If the herniated disc is lateral to the spinal canal, the disc herniation is removed from the side through a small window, in what is known as the lateral approach, using microsurgical techniques.
An artificial disc is usually only inserted in the area of the lumbar spine (lumbar level) or the cervical spine (cervical level) if disc-related back pain and spinal problems persist and possibly even worsen, despite conservative treatment measures such as physiotherapy and pain management with medication and are accompanied by paralysis and restriction of movement.
The implantation of an artificial disc is intended to eliminate disc-related back pain and preserve the natural mobility of the spine.
AFTER SURGICAL TREATMENT AND REHABILITATION
The inpatient stay after surgery is usually about two to five days. If a drainage tube is placed, it will be removed the next day. Physiotherapy with back training begins on the first postoperative day. For the first six weeks, a lumbar brace/cervical collar is recommended while walking/standing to help the weakened disc to heal. During this time, avoid driving as well as bending the upper body forward.
During their stay, our patients are given an exercise programme that their physiotherapist creates individually for them and that they carry out together. This consists of isometric muscle contraction exercises (tensing the muscles evenly) that activate the segmental stabilising muscles of the trunk. Thermotherapy can be used following intervertebral disc surgery, preferably with movement therapies.
Dr Alessandro Rustia (I) has many years of experience and is highly skilled in spinal surgery and pain management. We ensure rapid, expert assessment and consultation as well as treatment in line with the latest medical possibilities. Don’t hesitate to get in touch if you would like a second opinion.
Because the Pyramid Clinic is a private clinic, patients here require supplementary insurance. You will therefore need private or semi-private insurance for your treatment. If you have general insurance you can also be treated here if you opt to pay for an upgrade.