Symptoms | Prevention | Diagnosis | Therapies | Consultation
Osteoarthritis is a joint disease. It begins gradually and leads to the joint cartilage slowly wearing away. This results in inflammation of the joint with joint effusion, pain and restricted movement. Though all joints can be affected, it is primarily the knees, hips, shoulders, fingers and feet. It can also affect the spine. As the abrasion increases, so does the pain. One characteristic of osteoarthritis is start-up pain: This means that the pain is particularly strong after a rest phase (e.g. sitting or lying) and decreases with increasing movement. In the final stage the pain is permanent and joint mobility can be severely restricted.
![Osteoarthritis of the knee]()
Osteoarthritis of the knee
![Osteoarthritis of the hip]()
Osteoarthritis of the hip
![Osteoarthritis of the shoulder]()
Osteoarthritis of the shoulder
![Osteoarthritis of the fingers]()
Osteoarthritis of the fingers
How does osteoarthritis develop?
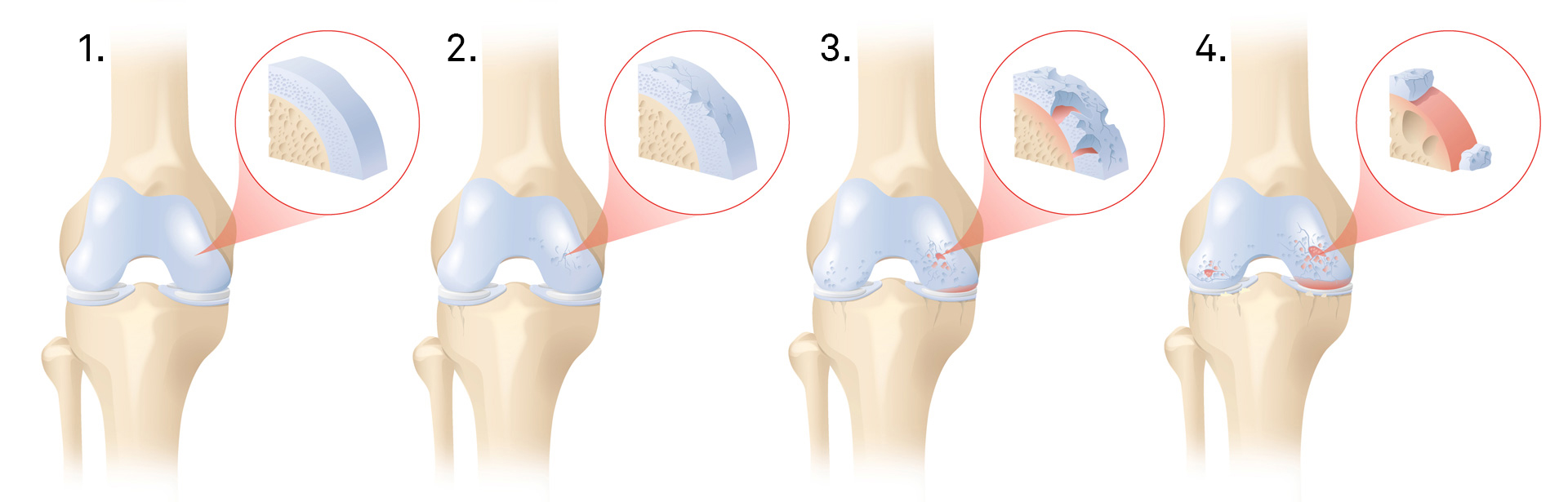
Osteoarthritis means a degradation of the joint cartilage. Everybody undergoes normal wearing of the joint cartilage during their life. In principle, osteoarthritis is divided into different stages:
- Stage 1: The cartilage softens.
- Stage 2: The surface of the cartilage becomes rougher and can be torn.
- Stage 3: The tears in the cartilage reach down to the bone.
- Stage 4: The cartilage is fully worn away and the underlying bone is exposed (“bone on bone”).
There are several causes for the gradual, mechanical degradation of the joint cartilage. These include a genetic (hereditary) predisposition, obesity, poor dietary habits or even too much or too little movement. The likelihood of osteoarthritis increases with age. The process can be accelerated if you are overweight or have had an accident. Stressful sports (especially stop-and-go) and arduous physical work also have an influence. Especially at risk are those who stress their joints constantly and extremely (such as professional athletes) or those who have suffered injuries with joint damage. It is not yet possible to cure the cause. Weight control and the avoidance of incorrect or excessive stress in sport or at work can slow the joint deterioration to a degree.
Osteoarthritis often develops gradually over several years. Over time, the joints affected by the osteoarthritis are no longer protected by cartilage. In contrast to cartilage, bone has pain receptors. Thus the stress-dependent joint pains which slowly grow stronger reflect the increasing exposure of the bone. Progression of the osteoarthritis typically leads to wave-like pain during stress and, later, to constant pain when resting, especially at night. The pain-free intervals become shorter as the osteoarthritis progresses. This is accompanied by inflammation and swelling of the affected joint, restricted movement, shortening of the musculature and deformation of the joint with increasing malformation up to complete restriction of mobility. The more painful it becomes, the less the affected joint is moved. This is a vicious circle as movement is highly important for the perfusion and regeneration of the cartilage.
A healthy lifestyle with appropriate nutrition, consumption of specific building blocks and mobility are fundamental for preventing osteoarthritis. When a joint is moved, it produces a lubricant called synovial fluid. This not only reduces friction, it contains nutrients for the cartilage. Regular movement and targeted exercise can build up the muscle around the joint to stabilise it. You should therefore stay active with sports as long as possible.
However, not all sports are equally suitable. Most ideal are sports which are gentle on the joints such as swimming, water gymnastics, cycling with low resistance or hiking on flat terrain. Specific medical exercise therapies (physiotherapy, pilates, AmpliTraining, etc.) can also be considered. Ball sports with rapid changes of direction and abrupt movements (stop-and-go) are not good and can even exacerbate the problem.
Unfortunately, it is still not possible to completely heal osteoarthritis. However, the right therapy and treatment methods can considerably relieve the pain and maintain the mobility of the affected joint for a longer time. It is also important to consult a specialist early. The earlier you act, the better the chances for a life and movement as pain-free as possible.
Strong joint pain with accompanying impairment or difficulties in everyday movements such as climbing the stairs can be an indication of osteoarthritis. Personalised questioning of the patient by the specialist regarding when and how the pains appear is followed by a comprehensive clinical examination of the affected joint to assess and localise the pain, movement restrictions, anatomical differences and muscle strength. A radiological investigation of the affected joint is then performed. If there is any uncertainty, an MRI (magnetic resonance imaging) can be performed to evaluate the cartilage situation better. Infiltration of the joint with anaesthetic can also provide information about the cause. Once all investigations are complete, the results are discussed with the patient and the next steps decided.
Treatment depends on the stage of the osteoarthritis, the degree of suffering and the patient’s needs. Treatment starts with conservative methods on principle. If the results of this are not satisfactory over the long-term, surgical methods should be considered and an appropriate specialist consulted.
Conservative treatment methods
- Physiotherapy: Targeted and repeated exercises improve coordination and increase endurance.
- Medications: Pain relievers and agents to support the cartilage
- Joint injections (cortisone, hyaluronic acid, autologous blood) against pain and/or to reduce inflammation and lessen joint pain.
- Inserts, knee bandages
Surgical treatment methods
Joint-preserving surgery:
- Joint imaging (arthroscopy)
- Repositioning (e.g. from bow legged to knock-kneed)
Artificial joint replacement:
Conservative osteoarthritis therapies in the form of medications, pain-relieving gels, cartilage-protecting substances, injection/infiltrations and medical exercise therapy should be preferred whenever possible and sensible.
MORE ON OUR TREATMENT METHODS
Our doctors have extensive experience and expertise in joint and sport surgery. With knowledge of the disadvantages which accompany referring out the treatment of acute and chronic pain of the locomotor apparatus, we provide rapid, expert investigation and consultation as well as treatment without delay.
You can also ask us to provide a second opinion.