Knee replacement | Artificial knee
Methods | Knee replacement | Knee replacements and allergies | Operation | Clinic stay | Rehabilitation | Costs | Consultation
When might I need a knee replacement?
The knee is a very complex joint. Damage within the joint, such as to the joint cartilage or the meniscus, can lead to osteoarthritis of the knee. This is often very painful, leading to a loss of mobility.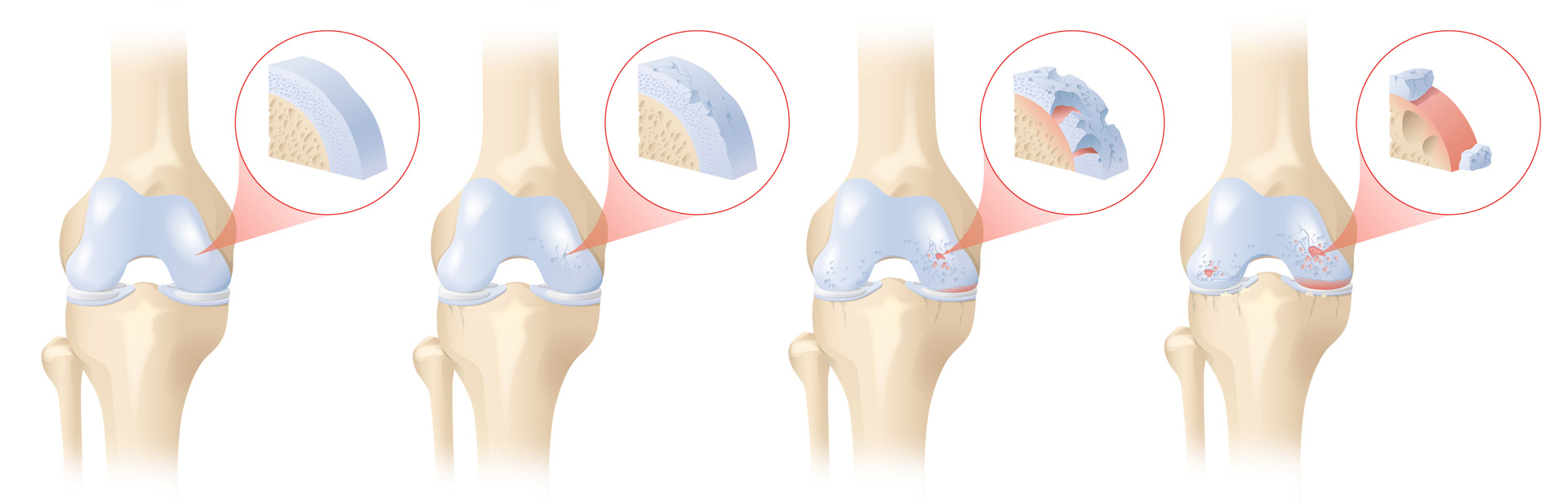
Advanced osteoarthritis of the knee often requires a partial or total knee replacement if symptoms have not been successfully alleviated by conservative treatment or by arthroscopy.
A thorough examination will determine if a knee replacement is appropriate and necessary in your case. The objective of a knee replacement is freedom from pain as well as restoration of the ability to move and walk. However, an artificial joint can never completely replace the perfection of a natural joint. One must always be aware that this is an artificial joint with mechanics that can sometimes be heard, and that it is subject to wear in proportion to the load placed on it. Before surgery, your specialist will explain the operation and the steps in the procedure. They will also explain what type of knee prosthesis should be implanted. However, the exact state of the joint only becomes fully visible during the procedure. It is therefore possible that at this time, deviations from the normal course of the operation as discussed with you may occur.
Watch the following video to learn how the Pyramid Clinic helped Violette Flückiger with a knee replacement operation (in German):
There are various methods available at the present time, but soft tissue-oriented knee joint resurfacing has proved particularly successful in knee replacement surgery. In this method, the collateral ligaments of the affected knee are given special attention. In contrast to other methods, in which computers or individual templates are used to ensure that the upper and lower leg axes are properly aligned (axis-oriented method), in the soft tissue-oriented method, the forces of the medial and lateral collateral ligaments in flexed and extended positions are determined during surgery using a special soft-tissue pressure sensor. Scarred collateral ligaments are released until the affected knee, under the same amount of pressure on the medial and lateral collateral ligament, is straight again. Thus it is possible to adapt the artificial knee joint resurfacing individually to the various illness-related changes in the knee joint. Only after the collateral ligaments are balanced and the leg is straight is the surface replacement inserted to form the “new cartilage”. This ensures that the new artificial knee surface replacement is evenly loaded.
The soft tissue-oriented method is used for the following procedures:
- Partial resurfacing (unicompartmental prosthesis, patellofemoral replacement): only one half of the joint surface needs replacing, thereby preserving the cruciate ligaments.
- Total resurfacing (knee replacement): the entire joint must be replaced.
- Revision knee replacement (interlocking/constrained knee prosthesis, total knee replacement): when the collateral ligaments no longer function or bone quality is poor (osteoporosis); in cases of significant malpositioning or as a replacement for an existing prosthesis.
![Partial resurfacing (sledge prosthesis)]()
Partial resurfacing (sledge prosthesis)
![Partial resurfacing (patellofemoral replacement)]()
Partial resurfacing (patellofemoral replacement)
![Total resurfacing (knee replacement)]()
Total resurfacing (knee replacement)
![Revision knee replacement]()
Revision knee replacement (interlocking/constrained knee prosthesis, total knee replacement)
What are the advantages of the soft tissue-oriented method?
The soft-tissue oriented approach that focuses on the collateral ligaments is gentler, less painful and promises better mobility and stability. Also, no blood donation is necessary prior to surgery. After surgery, the patient can immediately put weight on and move the operated knee. Contact us here for a personal consultation.
The type of knee replacement that is best suited to your individual case will be clarified during the preliminary consultations. However, the exact state of the joint only becomes fully visible during the procedure. It is therefore possible that at this time, deviations from the normal course of the operation as discussed with you may occur. You can find further information on choosing the right replacement joint in this article (in German). Contact us here for a personal consultation.
Normal knee replacements are made of stainless steel, an alloy containing a mixture of cobalt, chromium, molybdenum and nickel. Some people have a known allergy to these components, or can develop one over time. To prevent this, we use biocompatible, hypoallergenic prostheses whenever possible. These are sprayed with titanium, which makes the surface of the artificial joint even smoother. This results in less wear and smoother motion of the artificial joint. The titanium coating also prevents potential allergens such as nickel from dissolving out of the components. Consequently, we have less irritation of the tissue, less pain and a longer lifespan of the artificial joint. The components of the meniscus replacement (inlay) and the replacement of the posterior surface of the patella are made of a kind of plastic (ultra-high-molecular-weight polyethylene).
How can I prepare for the procedure?
There are several ways in which you can help to ensure that you will quickly be up and about after knee replacement surgery. Primarily, you need to be 100% sure that now is the right time for a knee replacement.
Muscle development and movement
It is important that you continue to bear weight and exercise your knee joints until the date of surgery, because the stronger your muscles and the better your mobility before the procedure, the faster you will be back on your feet. It takes three times longer to build muscle than to lose it. Having physiotherapy before surgery also provides positive support for your muscles. In addition, the preliminary exercises can show you how best to walk using walking sticks.
A strong immune system
Studies show that strengthening the immune system with additional vitamin and protein intake before and after surgery is extremely important in minimising the rate of complications. Well-tolerated dietary supplements are available for this purpose. Shortly before the procedure, we also recommend that you clean the skin area to be operated on with appropriate disinfectant wipes and/or a special shower gel. This helps to reduce the risk of infection.
A check-up with your GP is also important. Anaemia or other deficiencies (e.g. cardiovascular problems, coagulation disorders, etc.) should be ruled out before surgery and treated if necessary. Being very overweight or smoking is also unhelpful and you should therefore avoid this or work on reducing this.
Dental check-up
Before a major joint replacement operation, we recommend that you have a dental check-up and any necessary procedures. An appointment with your dental hygienist is also recommended before surgery. After surgery, you should not visit the dentist or hygienist for at least three months to avoid possible infection.
The procedure varies depending on whether it is a partial or total replacement or a revision knee replacement. However, the processes during surgery are similar. In the initial step, diseased bone and tissue are removed. The remaining bone is then shaped so that the components of the knee replacement fit exactly and can be fixed in place. For most of the procedure, a tourniquet is not needed. The form of tourniquet used for a small part of the operation is an inflatable cuff which is placed around the thigh and interrupts the blood flow to the leg. By doing without it, bleeding can be better controlled and the tissue protected. This improves wound healing and reduces the risk of infection. The tourniquet is only used when cementing the artificial joint, to ensure the best possible contact between the bone, cement and artificial joint.
You can find a detailed and illustrated description of the surgery in our patient brochure (in German). Contact us here for a personal consultation or find out more through our introductory video (in German):
What type of anaesthetic is used?
Knee surgery can be carried out under a general anaesthetic, regional anaesthetic or nerve block (anaesthesia near the spinal cord or local anaesthesia) or these forms of anaesthesia may be combined. Talk to your anaesthetist before surgery about which form of anaesthesia is best for you.
Orthopaedic surgery has made great progress in recent decades. When performed by an experienced orthopaedic surgeon with years of training, knee surgery is now a routine procedure. So as a patient, you don’t need to be afraid of surgery. Anaesthesia has also developed further and the anaesthetics used today are very well tolerated and safe, even during lengthy procedures.
But every operation involves risks. These include general complications such as: infections, problems with wound healing, bruising and bleeding, thrombosis, injuries to nerves, vessels or other anatomical structures, adhesions, excessive formation of scar tissue with reduced mobility and function of the knee joint and residual pain. Specific complications such as bone fractures, allergies, increased osteoarthritis behind the kneecap, suboptimal placement of the artificial components, incorrect alignment of the kneecap, etc. will be discussed with you in a detailed consultation.
During the initial surgery the risks are small, but they increase with each further procedure on the knee. Complications may mean that further surgery will have to be carried out. In a good clinic, you are under close supervision so that staff can react quickly in the event of complications.
The average stay at the clinic is one week. As early as the first day after surgery, your movement therapy and daily exercises can start. On approximately the fourth day, you will be able to walk a few steps independently on crutches. The affected leg can take your full weight if pain and swelling allow it. Walking sticks will be needed in the first four to six weeks, mainly for your safety and for gait training. You can continue to take painkillers for as long as you’re in pain. For six weeks you will need to take medication to prevent thrombosis. Stitches will be removed just under two weeks after the procedure.
Regular follow-up checks at our centre enable us to monitor the healing process and, if you wish, to provide our recommendations or other supportive advice for therapy, such as massage.
Sports activities or hobbies such as skiing or golf can also be resumed after a knee replacement (links are to articles in German). Building up the muscles is important.
Your stay in the clinic should be followed immediately by several weeks of physiotherapy. Most patients arrange matters in such a way that they visit our physiotherapy team two to three times a week, but of course it’s possible for you to visit a physiotherapist near your home. We’re happy to provide you with details of the appropriate requirements. Some health insurance providers also cover inpatient rehabilitation or convalescence. Only make plans for this after clarifying your situation well in advance. If you want or need to have help at home, you may be able arrange Spitex home care. We are happy to help you with the arrangements. You can find information on practical exercises to do at home here (in German).
How long does a knee replacement last?
Although you might hope that the new knee will last a lifetime, it is important to be aware that an artificial knee joint is always a temporary solution: not because of the prosthesis itself, but because the ageing process can have a major influence on the stability of the artificial joint. These days, the average lifespan of a prosthesis is at least ten to fifteen years. This means that patients who have a knee joint replacement at a young age can expect to need another replacement or revision procedure later in life. However, given the remarkable progress in surgical techniques and the development of new artificial joints, this need not be seen as a problem. The lifespan of an artificial knee joint can be negatively affected by many factors. Ultimately, this leads to a loosening of the artificial knee joint with an associated increase in pain upon weight bearing and gait insecurity. At an advanced stage, this requires a revision knee replacement.
Stress on the joint
Increased stress on the artificial joint and a deterioration in the original anchoring of the joint within the bone are the mechanical causes that negatively influence the lifespan of an artificial joint. Your own activity levels play an important role in how much stress is placed on the joint. The more active you are and, above all, the more sports that you do that stress the joints, the more the anchoring of the lower leg bone is stressed by the artificial joint. Excess stress can also occur if the artificial joint is not optimally positioned. Furthermore, the original anchoring of the artificial knee joint within the bone may deteriorate: slowly due to an increase in osteoporosis or rapidly due to a bone fracture following a fall. Both lead to loosening of the artificial knee joint.
Infection
Infections trigger the immune system, causing inflammation and weakening of the anchoring. Any infections can be a threat for your artificial knee joint throughout its lifespan. Bacteria can enter the bloodstream via wounds to the skin or the mucous membranes, or via lung or bladder infections, etc. and then settle in the artificial knee joint. They may multiply there, leading to an infection. However, this happens gradually, meaning that the infection is only detected after a long time has elapsed. When it finally becomes apparent, it is primarily through severe pain and swelling.
Allergies
Allergies can develop over the course of a lifetime. This can happen when the immune system defends itself against the foreign bodies, consisting of stainless steel (nickel, chromium, cobalt and molybdenum) or bone cement. The result is a non-infectious inflammation of the artificial joint with resulting loosening of the joint.
New occurrences of pain in the artificial knee joint triggered by weight bearing or movement should definitely be checked by an experienced knee specialist if they do not resolve within a short time.
Living with a knee replacement
After the operation and subsequent rehabilitation, you should not only be free of symptoms, but also be more or less able to live your life and pursue your favourite activities as before. This includes social and sporting activities. If you have adjusted well to the new joint, increased your training moderately and not taken too many risks, all types of sport should be possible again. Of course, some sports such as skiing, snowboarding, football, tennis (stop/start, contact sports, etc.) are more dangerous and less suitable than gentler sports such as swimming, cycling and hiking.
One thing to bear in mind is that you should take special care when visiting the dentist. The mouth contains many bacteria, which normally do not cause problems. However, if you have an injury to the mucous membrane or if you have tooth decay that develops into an abscess, oral bacteria can enter the bloodstream. Not only do these weaken the immune system but they are also deposited within the artificial knee joint after surgery, where they can multiply. This can cause an infection in the artificial knee joint. It is rare for an infection of the artificial joint to be caused in this way, but it can result in serious complications for the person affected. The infected artificial joint will need surgery and a long course of antibiotics is required to support recovery. If treatment does not work, the artificial knee joint must be completely removed, and at a later point in time – when the joint infection has healed – a new knee replacement must be fitted. This can be problematic, both mentally and physically. In addition, the outcome in this situation is usually worse, and is associated with more pain and less mobility. Good oral and dental hygiene is therefore highly recommended.
In an emergency or in the event of other surgery, treatment with prophylactic antibiotics should generally be considered, depending on your state of health (immunosuppression, diabetes mellitus, etc.) and the nature and duration of the procedure. You should let your doctor know that you have an artificial joint.
The cost of knee surgery depends on various factors, but mainly the duration and complexity of the procedure and the size of the artificial joint to be implanted. Your health insurer will normally bear the full costs, if you have the appropriate policy. For treatment at the Pyramid Clinic you will need supplementary private or semi-private insurance.
Ideally, you should clarify with your insurer before surgery as to whether they will also cover a subsequent rehabilitation stay.
If you want to pay for the procedure yourself, we will be happy to prepare a cost estimate on request after a detailed examination. This can be especially helpful for international patients.
Our doctors have many years of experience and are highly skilled in sports and joint surgery. Dr Andreas L. Oberholzer is a well-known expert in knee surgery and has extensive experience in knee replacements. He trains international doctors in this area and promotes the further development of soft tissue-oriented techniques for implantation of artificial knee joints. You can find out more about his work here.
We guarantee rapid, expert assessment and consultation and treatment in line with the latest medical findings. Don’t hesitate to get in touch if you would like a second opinion.
Please note: Because the Pyramid Clinic is a private clinic, patients here require
supplementary insurance. You will therefore need private or semi-private insurance for your treatment. If you have general insurance you can also be treated here if you opt to pay for an upgrade.