Osteoarthritis of the hip (Coxarthrose)
Cause | Symptoms & pain | Diagnosis | Conservative treatment methods | Surgical treatment methods
When the actual stress on the joint cartilage is higher than its genetical capability can withstand, the joint cartilage is worn down. A lasting imbalance leads to osteoarthritis of the hip, also called coxarthrosis.
The actual stress on the joint is increased by obesity, accidents, congenital malformations (hip dysplasia), natural ageing (loss of the cartilage’s elasticity and ability to store water) and jobs or sports, that strain the joints. All those things lead to a loss of cartilage, which promotes arthrosis.
We differentiate four stages of osteoarthritis. In the first phase there are only a few small tears on the surface of the cartilage. In the last stage most of the cartilage is worn off completely, so the rough, painful surface of the bone is exposed.
Cartilage damage is divided into four stages:
 Stage/Grade I: Soft cartilage
Stage/Grade I: Soft cartilage
Stage/Grade II: Rough surface with tears
Stage/Grade III: Deep tears in the cartilage down to the bone
Stage/Grade IV: Complete depletion of the cartilage with exposed bone: this is known as bone on bone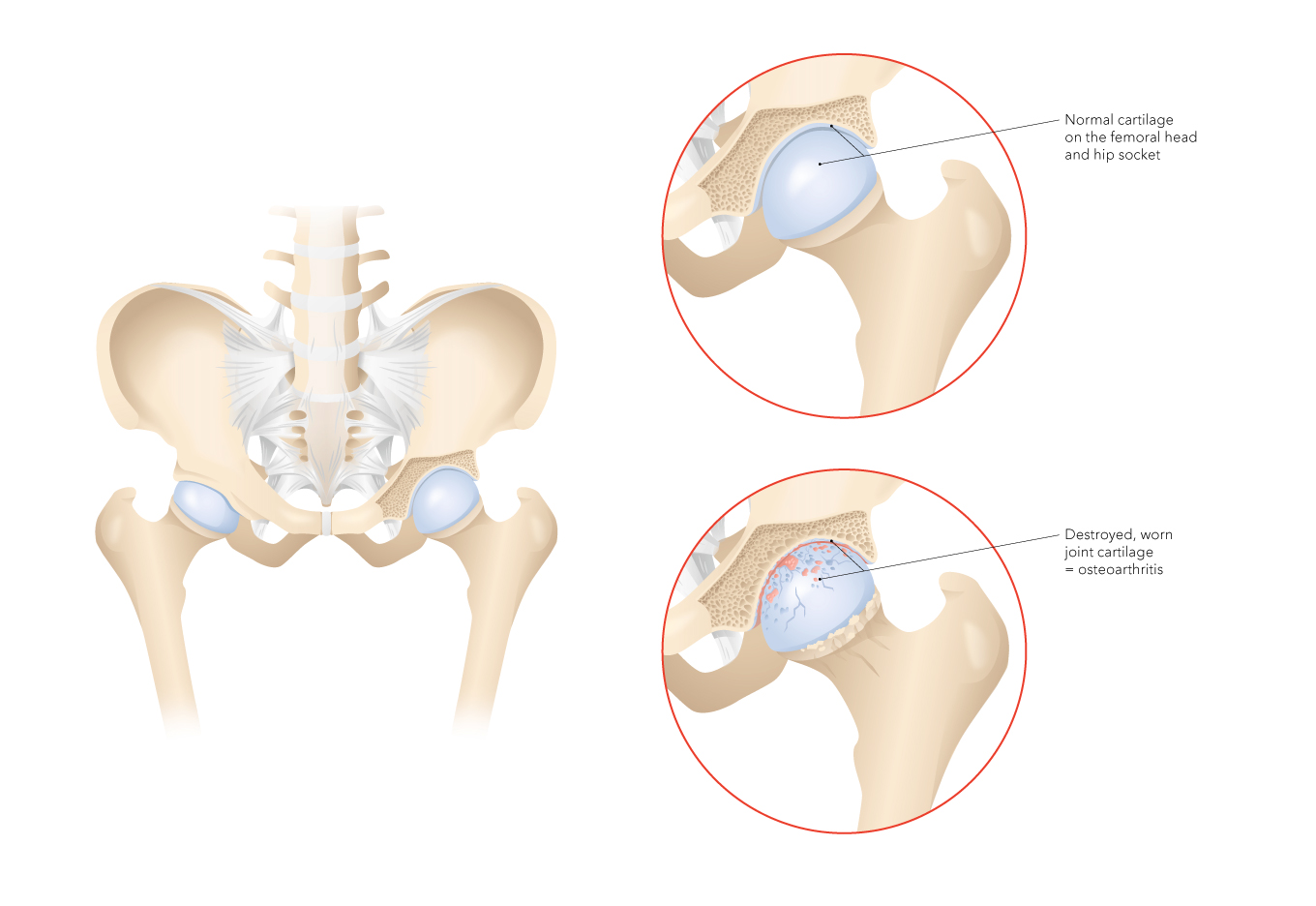 In comparison to bones, cartilages contain no pain fibres (nerves). Therefore, the damage of the cartilage is only notices when the deterioration reaches the bone.
In comparison to bones, cartilages contain no pain fibres (nerves). Therefore, the damage of the cartilage is only notices when the deterioration reaches the bone.
If you suffer from ongoing pain due to osteoarthritis of your hips, and all conservative treatments have failed, you might want to consider a hip replacement.
The aim of an artificial hip is the absence of pain and the improvement of mobility. Artificial hips come in various sizes and different materials. However, an artificial joint can never fully match the perfection of a natural joint.
Learn more about osteoarthritis.
Osteoarthritis of the hip may be experienced differently by each person. For most patients, various hip joint pains (pain when initiating movement, when bearing loads or inflammatory pain) and restrictions in the mobility of the hip are the primary focus.
Start-up pain
In the final stage of osteoarthritis, the bone is no longer covered by the protective, smooth cartilage. The exposed joint bone has a rough surface. If two rough joint surfaces come into contact, they interlock. This causes blockage of the joint. This blockage must be released by an initial movement. This breaks the delicate bony connections, causing the typical start-up pain which then passes again after a few steps.
Stress pain
Another pain typical for osteoarthritis is stress-related pain, felt as a dull ache around the hip joint, partially radiating into the upper thigh. In contrast to the cartilage, the exposed bone in the joint possesses pain fibres. These are activated when bearing loads.
Inflammation pain
A further pain typical of osteoarthritis can be caused by inflammation of the joint. This arises through continual rubbing of the rough surfaces. Think of sandpaper. This exposes abraded cartilage and bone which irritate the mucosa (synovium) of the joint. This leads in turn to increased production of joint fluid, effusion, overheating and pain which gradually worsen.
Restriction of movement
In the final stage of osteoarthritis, the bone-forming cells of the exposed bone are stimulated by the pressure and the cartilage-bone abrasion. The activated bone cells build new bone to distribute the pressure over a larger area. However, the newly formed bone is soft and may lead to a deformation of the hip joint with resulting restrictions of movement. The joint thus grows gradually stiffer. These restrictions of movement lead to increasing difficulty with everyday activities such as: Pulling on socks and shoes, cutting toenails or climbing into the car.
The following additional consequences can occur in advanced osteoarthritis of the hip:
- Deformation of the joint (shortening of the leg ➞ pelvis obliquity ➞ back problems)
- Unstable gait with a risk of falling
- Restricted movement (e.g. difficulty pulling on socks/stockings)
- Muscle tension, muscle shortening and muscle weakness
Strong hip joint pain, restricted hip movement and increasingly unstable gait with resultant risk of falling must be investigated carefully. After questioning the patient personally regarding when and how the pain occurs, there is a comprehensive clinical examination of the hip joint to assess and localise the pain, movement restrictions, differences in leg length and muscle strength.
This is followed by a radiological examination of the hip joint. In the event of uncertainty, MRI (magnetic resonance imaging) can also be performed to assess the cartilage situation in the hip joint better.
When all examinations have been completed, the results are discussed with the patient in detail, potential therapies explained and the next steps decided.
WHAT THERAPIES EXIST FOR OSTEOARTHRITIS OF THE HIP?
If the osteoarthritis of the hip joint is not yet too advanced, it can be treated with shoe inserts, shoes with cushioning soles, walking sticks, physiotherapy, medications against the inflammation and pain as well as cartilage-supporting medications or dietary supplements. Lifestyle changes may also be required with respect to food and sports which are gentler to the joints (hiking, swimming, cycling, etc.). It is important to keep the arthrotic joint in motion with sports such as cycling, swimming, etc. which do not overly stress the joints.
Weight reduction is of course helpful in the event of obesity. Otherwise, injection of lubricant, injection of cortisone may help to reduce the arthrosis pain.
Overview of the conservative treatment methods available:
- Anti-inflammatory and pain-relieving medications
- Medications and substances (dietary supplements) to strengthen the cartilage
- Medical training therapy /physiotherapy
- Injections of lubricants into the joint (hyaluronic acid) and anti-inflammatory medications (cortisone)
- Aids such as walking sticks, inserts, orthopaedic shoes
- Lifestyle changes in regard to sport, obesity, diet, etc.
These measures can help to reduce the pain of osteoarthritis and slow the progression of the cartilage abrasion. However, the osteoarthritis itself cannot be stopped or corrected by these conservative measures.
Injections into the hip joint are performed under X-ray or ultrasound for control as the hip joint is well packed by the surrounding musculature and enclosed in a tough joint capsule. This technical support is required to ensure that the syringe does indeed enter the hip joint and delivers the contents to the affected hip. We therefore work with a radiology centre which administers the appropriate injections.
Injections with hyaluronic acid
The hyaluronic acid product is a synthetic lubricant manufactured for joints. These injections into the joint reduce the abrasion of the arthrotically changed cartilage surfaces. The joint can then move better. In addition, the lubricant means the joint is less irritated, reducing osteoarthritis-related joint inflammation, which reduces the osteoarthritis pain in turn.
The effectiveness of the lubricant injections is dependent on the stage of the osteoarthritis. Many patients recover a good quality of life thanks to these lubricant injections. Initially, three injections of lubricant are given overall, at intervals of one week. As these require X-ray or ultrasound support, the injections are administered in a radiology centre. The effect of the lubricant injections persists for a certain time. If the response is good, the injections can be repeated at any time.
The costs for this treatment are not reimbursed by health insurance. The price for a lubricant injection to treat osteoarthritis of the hip is around CHF 130.
Injection of cortisone
Cortisone is made in our own bodies and used to relieve inflammations (among other things). This property is exploited. The synthetic cortisone is injected into the affected joint. This cortisone dissolves slowly and thus has a longer effect, temporarily relieving the osteoarthritis pain. Unfortunately, cortisone also has side effects. It attacks the bone and cartilage and weakens the tendons. Cortisone also suppresses the body’s immune system, increasing the risk of infection. Despite the local injection of cortisone into the joint, a portion of this can also enter the circulation and trigger corresponding, temporary effects. We therefore administer the cortisone injection with great caution.
So that the contents of the cortisone injection correctly enter the affected hip joint, this requires support with either X-rays (image converter) or ultrasound. We therefore work together with a radiology centre.
If hip problems persist despite these conservative measures and the quality of life suffers accordingly, it is time to consider a hip replacement (artificial hip). Thanks to minimally invasive surgical methods which protect the muscles, the new artificial hip is implanted from the front to protect the tissues. The stabilising hip muscles are simply pushed to the side, not partially cut through, as previously. This has the advantages that there is less pain, less blood loss and reconvalescence can be faster. This can increase the quality of life immediately.
We will be pleased to give you a private consultation
Our doctors have extensive experience and expertise in joint and sport surgery. PD Dr Andreas L. Oberholzer is a certified hip expert with broad experience in the field of osteoarthritis of the hip.
We guarantee a fast, specialist investigation and consultation as well as treatment with the latest options. You can also ask us to provide a second opinion.