Preparation | Surgery | Follow-up | Risks | Consultation
WHAT IS THE OPTIMAL TIMING?
The restriction of the quality of life caused by advanced osteoarthritis of the hip has different impacts on each person. The decision to operate must be right for you. You determine when it is the right time for an artificial hip. Unfortunately, the wearing of the cartilage caused by osteoarthritis increases exponentially. This means that the hip pain and restrictions of movement, instability and risk of falling will increase with time unless the problem can be stabilised - at least partially - at an early stage with targeted increases in muscle strength. The more pain, though, the less you want to use your muscles. This is a vicious cycle as it leads to weakening of the muscles. Unfortunately it also the case that muscles degrade much faster than they are built up.
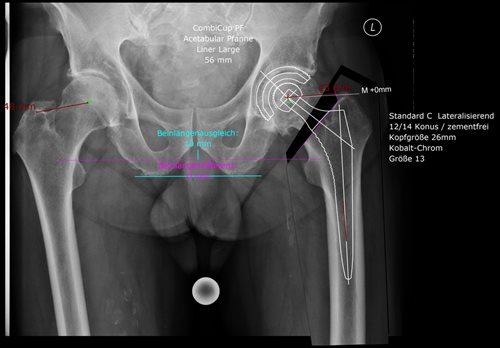
Each hip surgery is individually planned by the surgeon before the operation. This requires a current X-ray of the pelvis with a reference sphere (usually a 2.5 cm metal ball). Using the reference sphere and an appropriate planning program, the size of the hip shaft and socket can be determined precisely and individually on the corresponding X-ray image.
HOW CAN I PREPARE MYSELF FOR THE PROCEDURE?
Before the surgery, you can also help ensure the operation will be successful with rapid improvement after implanting the artificial hip.
The most important prerequisite is that you are 100% convinced it is the right time for you for an artificial hip and that you feel well supported and understood by your doctor. Only together can we achieve a good result.
Healthy lifestyle and training
An unhealthy lifestyle (especially smoking) and obesity can impair the chances of healing. Strong smokers usually have worse blood perfusion and wound healing. Being overweight places additional stress on the joints and makes mobility and strength training after the surgery more difficult.
To prepare for the surgery, we recommend that you keep moving and training your hips despite the pain: the stronger the muscles and the better the mobility before the surgery, the faster you will be back on your feet. You need at least three times longer to build up muscle than for it degrade. Good nutrition and high-quality protein also support the growth of the muscles. Physiotherapy before the surgery can support this and prepare you for the time after the operation.
Strengthening the immune system
As already shown in several studies, strengthening the immune system with sufficient vitamins and proteins before and after the surgery is enormously important for minimising the rate of complications. Well tolerated dietary supplements help in this regard.
Our skin is our natural protection against the outside world and is home to several different skin bacteria. These are normally harmless. However, in the event of a skin injury and weakened immune defences they can lead to infections. We therefore recommend our patients independently cleanse the entire body with a special washing lotion for five days before the surgery and disinfect the area of skin to be operated on with appropriate disinfectant cloths. These measures can significantly reduce skin bacteria and lower the risk of infection.
Check-up at the GP and dentist
We also recommend a check-up at the GP so that anaemia, a tendency to bleed or heart problems can be excluded or, if required, treated before the procedure. As all these measures have a positive effect on the result of the surgery, we specifically instruct our patients on these points before a major operation, such as an artificial knee or hip (pamphlet, consultation, product recommendations, etc.)
Before major joint surgery we also recommend a dental check-up and to have the teeth cleaned if necessary. Dental hygiene (DH) is also recommended before the procedure. After the surgery, you should not got the dentist or dental hygienist for at least 3 months to avoid possible infections.
So that surgery to implant an artificial hip with the more modern minimally invasive and tissue-sparing technique from the front is successful, it is made under general anaesthetic, guaranteeing the optimum muscle relaxation.
1. Illustration of the hip joint
For the minimally invasive, tissue-sparing access to the hip joint from the front, an around eight centimetre incision is made in the skin of the exterior groin. The stabilising hip muscles are pushed carefully to the side, exposing the affected hip joint. The anterior joint capsule is then removed and the diseased, osteoarthritically worn hip joint becomes visible.
2. Removal of the femoral head
A saw is then used to separate and remove the worn femoral head and a part of the femoral neck. The shaft model being used determines whether more or less bone is removed from the neck of the femur. After removal of the worn femoral head, the joint socket is visible.
The new artificial hip joint is then reconstructed.
3. Preparation of the hip socket and its replacement
Special mills in different sizes are used to prepare the hip socket. These special hip mills free the natural joint socket from the old capsule and cartilage tissue until well perfused bone tissue is visible. The size is controlled using imaging (X-rays during the surgery). The well perfused bone tissue ensures firm fixation of the new artificial hip socket. The new, definitive hip socket and corresponding inlay as a replacement for the cartilage are then implanted.
4. Preparation of the femur and placement of the shaft
The femur is a long bone. Its exterior is a strong layer of hard bone (cortex). The hollow interior of the femur (medullary space) is soft and filled with delicate bone trabeculae (spongiosa). This interior is then prepared with special shaft files of different sizes. If the grip and size are good, which are also controlled by X-ray, a trial repositioning of the hip follows. This tests the stability of the hip and which movements might dislocate it. If the muscle tension is too low and the hip joint dislocates easily, either the femoral head is lengthened or the shaft enlarged, even if this might lead to lengthening the leg. The stability of the new hip joint is more important than achieving symmetrical leg length. Once everything has been checked and inspected, the sample parts are removed and the definitive parts of the new hip replacement are put in place. If the bone quality does not allow for cement-free fixation, the new artificial shaft must be cemented in.
5. Repositioning of the new artificial hip
After the new hip socket, socket inlay and shaft have been implanted and the definitive head of the femur has been adjusted to the correct size and length, the artificial hip joint is repositioned. This restores the movable connection between shaft and socket. After a further functional control, an X-ray is taken of the new hip joint to control the definitive length of the artificial hip joint conclusively.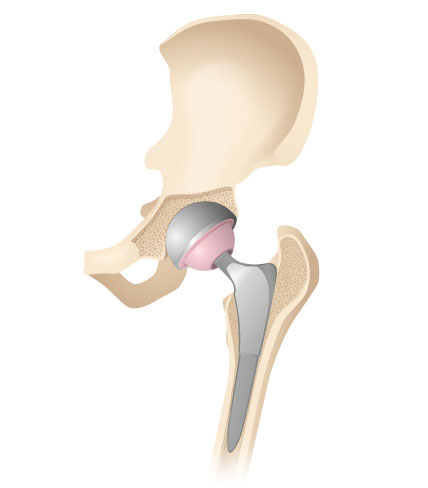
6. Close to the skin
At the end of the surgery, any bleeding is stopped and a drainage line is placed in the joint to channel away future accumulations of blood. The surgical wound is sewn back together in layers and covered with a sterile silicon dressing.
Facts and figures
![Operation]()
Operation
Surgery lasts between 1.5 and 2 hours, under general anaesthetic
![Operation]()
Length of stay at the clinic
Hospitalisation in the clinic for around 5 days
![After the treatment]()
After the treatment
![Back to work]()
Back to work
Depending on the activity, 4 to 6 weeks
You will stay in the clinic for around five days after the surgery. If a drainage tube has been placed, this will be removed on the next day. Physiotherapy within the clinic with walking training begins the day after the surgery. You should only partially load the operated hip by using a walking stick for around six weeks; this spares the soft tissues and supports the ingrowth of the bone into the new, cement-free artificial hip. Walking sticks give you stability and also help those around you to treat you thoughtfully. If the new hip has been cemented in place, it can be fully loaded on the next day. Nonetheless, we recommend you also use walking sticks for at least 14 days in this case. As the anterior capsule of the hip joint is partially removed during surgery, you must not rotate the operated leg externally, overextend it nor cross your legs for six weeks. This prevents possible dislocation of the hip joint. Dislocation of the hip - also called hip luxation - is an emergency, but luckily very rare. This usually happens by tripping, when the operated leg gets caught or through performing an incorrect movement. If this happens, the leg can no longer be moved or stressed and the leg shortens immediately. The hip must then usually be repositioned under general anaesthetic. However, follow-up surgery may also be required if something breaks or subsides during the dislocation or repositioning.
As the anterior capsule of the hip joint is partially removed during surgery, you must not rotate the operated leg externally, overextend it nor cross your legs for six weeks. This prevents possible dislocation of the hip joint. Dislocation of the hip - also called hip luxation - is an emergency, but luckily very rare. This usually happens by tripping, when the operated leg gets caught or through performing an incorrect movement. If this happens, the leg can no longer be moved or stressed and the leg shortens immediately. The hip must then usually be repositioned under general anaesthetic. However, follow-up surgery may also be required if something breaks or subsides during the dislocation or repositioning.
After six weeks, the joint capsule has regenerated and the three forbidden movements are slowly permitted again. Likewise, you should sleep on your back with pillows under the hollow of the knee for six weeks. The sutures are removed after 14 days.
Several weeks of physiotherapy should take place directly after hospitalisation. Most patients organise themselves so that they come to our physiotherapy department two to three times per week. However, you can of course choose another therapist closer to your home. We will be happy to issue the appropriate prescriptions. Certain health insurers will also reimburse in-patient rehabilitation or a stay at a health spa. This should be clarified in advance and only planned with the appropriate coverage. If you need or want assistance with the household, this can be organised through Spitex. We will be happy to help you with the organisation. Practical exercises at home and further information regarding out-patient physiotherapy, health spas or in-patient rehabilitation can be found here.
The implantation of an artificial joint is a routine procedure for the experienced specialist. Artificial joints have been tested and developed for many years and the corresponding surgical techniques have been optimised and refined constantly. In most cases, very good results can be achieved without work-arounds. However, you must be made aware that you are receiving an artificial joint. This may indeed be a replacement for a natural joint but in the end it remains a foreign body which may cause you problems.
Each surgery contains risks and something unwanted can happen at any time. The rate of complications during an initial procedure is relatively low, at one percent. However, the risk increases with each further operation. A good general health condition and healthy lifestyle help to minimise the risks. We differentiate between general complications which can occur during any procedure (e.g. infections, blood clots, nerve/muscle/vessel damage, postoperative bleeding, wound healing disorders or sensory disorders of the skin) and specific complications which can occur with regard to the artificial hip joint. These include:
- Early loosening of the fixation of the artificial hip joint to the pelvis (socket) or femur (shaft), with potential suspicion of a special infection
- Dislocation of the joint (luxation) with injury to the joint and/or fixation
- Differences in leg length, incorrect positioning of the axis and rotation errors of the leg
- Restricted movement owing to scarring and adhesions or impingements of tissues
- Allergy to the cement and/or prosthetic material
The risks are small during the initial procedure but increase with each further operation. A complication can lead to you requiring a further operation. In a good clinic you are monitored closely to allow rapid reactions to complications.
We will be pleased to give you a private consultation
Your well-being and personalised treatment are the focus at the Pyramid Clinic.
As the Pyramid Clinic is a private clinic, supplemental insurance is required: Treatments in our clinic require private or semi-private insurance. Naturally, we can also treat patients with general insurance if they opt for an upgrade.
Our experienced specialists will give you a personal consultation. Please contact us for more information or schedule an appointment directly: