Osteoarthritis of the end joint of the finger (Heberden’s nodes)
Causes and symptoms | Diagnosis | Conservative treatments | Surgical treatment | Joint replacement vs. fixation
The hands are more than just tools – they have a significant interpersonal function as a means of communication. When we meet, we pay particular attention to the unclothed areas of the other person – the face and hands. As well as eye contact, a handshake gives an immediate impression that can elicit sympathy or antipathy. People who interact with others regularly may be ashamed of the knotty appearance of osteoarthritis of the finger joint known as Heberden’s nodes. They may hide their hands in their pockets or close their fists in order to hide their fingers. Some people may go as far as to keep their hands under the table.
The deformation of the fingers and the increasing pain are due to the development of osteoarthritis of the finger joints. Unfortunately, this can run in the family. This tendency is usually passed on from mother to daughter; with sons affected to a lesser extent. Less commonly, this wear and tear on the joints can be caused by chronic strain, such as in massage professions or following injuries. Episodic pain is often the first symptom, sometimes long before changes can be seen on an x-ray. Over time, it can become increasingly difficult to close the fingers into a fist in the morning. These symptoms can get worse when it is cold and wet. As time goes on, knotty humps form on the backs of the end joints of the fingers, making the osteoarthritis visible to everyone. If the fingers then become crooked, stiff and misaligned from their axes, there is increasing functional restriction. Cysts can develop over the affected joints in different stages of the formation of osteoarthritis. These can cause unsightly furrow-like nail growth disorders due to the pressure on the fingernail growth zone.
If these changes become disturbing, a hand surgery consultation is advisable. The function is then thoroughly tested and, if necessary, the situation in the joint is investigated with an X-ray.
Conservative treatment
If the cartilage and bone changes are not very advanced, the symptoms can be treated with conservative rather than surgical measures. This includes protection from the cold, the use of cartilage-protective agents, pain relief ointments or sprays and cortisone injections if needed. If the pain is not sufficiently relieved, surgical treatment should be discussed.
Surgical treatment
If there is significant restriction of mobility, i.e. stiffening, and the finger is noticeably crooked, the only solution that can be offered is the removal of the destroyed joint and stabilisation, usually by means of a screw. In this case, pain relief can often only be reliably achieved at the expense of low mobility. However, the finger will be about 3 millimetres shorter. This surgical procedure is chosen exclusively for the treatment of pain. On the other hand, if you find the gnarly appearance of the arthritic finger aesthetically disturbing, the damaged joint can be replaced with a prosthesis earlier in the course of the disease if the function and axis are correct. With the insertion of an artificial joint, painful rubbing of the bone is prevented and mobility can be maintained. To do this, the extensor tendon is detached from the bone above the joint, bone growths of the arthritic joint and the damaged articular surfaces are removed and then the prosthesis is inserted. This is not anchored or cemented in the bone. Instead, it serves as a movable placeholder to prevent bone from rubbing against bone. A silicone hinge prosthesis is used in most cases. This type of implant has been used for decades.
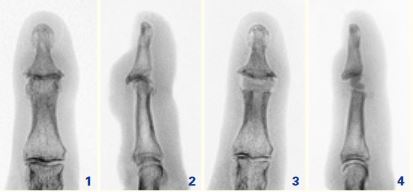 Fig. 1 and 2: Advanced osteoarthritis of the end joint of the finger (Heberden’s nodes).
Fig. 1 and 2: Advanced osteoarthritis of the end joint of the finger (Heberden’s nodes).
Fig. 3 and 4: After replacement of the joint. This case is ideal for prosthetic treatment because the finger axis is preserved, i.e. no deformation has occurred yet.
There are also artificial joints made of newer materials such as pyrocarbon. However, long-term clinical results are not available for prosthetics made from these materials. The procedure takes about 45 minutes per finger joint and can be carried out under local anaesthetic if preferred. Surgery can also be carried out on several fingers at the same time. If required, any joint cysts are removed and the narrower shape of the finger joint is restored. If the pressure of a cyst is removed from the nail growth zone, the furrow-like change to the nail grows out. However, it takes up to six months for the fingernail to fully recover. It is important to allow complete healing of the reattached extensor tendon over the artificial joint, which takes six weeks, in our experience. During this time, a small finger splint is worn, which only immobilises the joint that has been operated on. The function of the hand is not significantly affected.
If a joint with osteoarthritis is painful but functions well, fixation to relieve pain is not generally advised. In this situation, attempts are made to exhaust all conservative measures until the pain has increased so much that surgical treatment must be considered. However, if the mobility of the joint can be maintained by means of a joint replacement, this painful period can be shortened, and relief is possible at an earlier stage of the osteoarthritis. This avoids the development of deformation of the fingers. In addition, the finger length is retained with prosthetic replacement of the end joint. Any shortening due to fixation – and thus a certain inelegance – becomes unnecessary. In most cases, the wounds can be closed with a special wound plaster, resulting in almost invisible scars. As such, it would be possible to move the new joint immediately. However, the soft tissues around the joint replacement must first heal, especially the extensor tendon, which has been cut and reattached. If the postoperative immobilisation is insufficient, an extension deficit remains. This means that the finger cannot be stretched out completely straight. The duration of treatment does not differ significantly from that of fixation. As with all joint replacements, the bone around the artificial joint can break down and the prosthesis can loosen or break. If this complication occurs, it is still possible to switch from a joint replacement to fixation. However, if someone has to carry out heavy manual work that requires a lot of hand strength, stabilisation by means of fixation is recommended at the expense of mobility.
In summary, it can be said that prosthetic treatment of the end joint of the finger that has been damaged by osteoarthritis has a clear advantage over joint fixation in earlier stages of the disease. Mobility can be maintained in this way with reliable relief of pain, and the finger regains its normal appearance. This means that individuals do not have to endure pain until it is relieved by fixation. Instead the finger function can be preserved while taking aesthetic considerations into account.
Author: Dr Boris J. Czermak, FMH Specialist in Surgery, specialist field: Hand surgery
FACTS AND FIGURES
![SURGICAL PROCEDURE]()
SURGICAL PROCEDURE
1 hour, under general or regional anaesthetic
![SURGICAL PROCEDURE]()
HOSPITAL STAY
![AFTER THE TREATMENT]()
AFTER THE TREATMENT
Immobilisation for around 4 weeks, then increasing use possible
![TIME OFF WORK]()
TIME OFF WORK
![Sport]()
Sport
Resume after 6 to 8 weeks
![READY TO SOCIALISE]()
READY TO SOCIALISE
![COSTS]()
COSTS
Cost coverage must be requested from your health insurance company